Practical Information on Surgical Mesh
Practical Information on Surgical Mesh: what do I need to know?
by Charlotte Korte
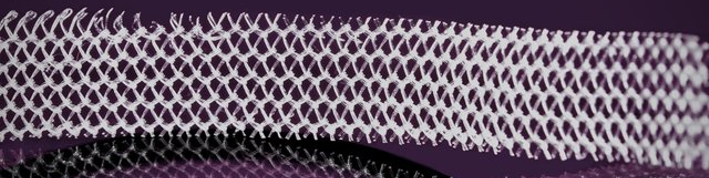
What products are known as surgical mesh?
The terminology that health professionals use to describe surgical mesh differs, so it is important to know what type of mesh is being implanted and if this is a synthetic polypropylene mesh (plastic).
|
|
|
The most common mesh used is non-absorbable mesh. This remains in your body indefinitely so should be considered a permanent implant. It is difficult to remove once implanted so this needs to be taken into consideration before consenting to mesh surgery. Synthetic mesh is used to treat stress urinary incontinence, rectal, bowel, vaginal, uterine and bladder prolapse and for hernia repairs. Both men and woman can be affected by mesh complications. Hernia mesh adverse events may not be as common as pelvic mesh related complications, yet if experienced can also be severe.
Although other products can be used in surgical procedures to treat these same conditions, this document primarily focuses on polypropylene (plastic) mesh.
Recognising the symptoms of surgical mesh complications
Not all who have surgical mesh implanted will experience complications, but as symptoms can present many years later it is important to know what to look out for. The list below is not conclusive; a more comprehensive list of potential adverse events associated with mesh related symptoms is at the end of this document, in Appendix One.
- Pain – (which can be acute) including referred pain down leg, buttocks, sacral and back, tailbone, groins, vagina, bladder/bowel, pelvic, lower limb, pain before/during and after bowel Pain can present in various ways from a slow burning pain, intense pain, to short stabbing pain sensations.
- Recurrent urinary tract infection.
- Infection.
- Discharge (vaginal or rectal).
- Difficulty urinating, also known as voiding dysfunction (Dysuria).
- Bleeding.
- Pain during sexual intercourse (dyspareunia).
- Painful sex experienced by the man – men may feel the mesh during sexual intercourse (hispareunia) – although not as common.
- Onset of auto-immune disorders.
- Impact on quality of life, sitting, standing, walking, and functioning in everyday activities.
- Nerve neuralgia – a stabbing, burning, and often severe pain due to an irritated or damaged nerve.
Surgical mesh device implants have been known to cause erosion where mesh pushes against/into the surrounding tissue, nerves, and organs. Although not as common, mesh can cause extrusion, where mesh pushes through or perforates surrounding tissue, nerves, and organs. Mesh is no longer thought of as inert; research has shown after implantation over years the mesh material can break down, shrink, and change over time. The formation of excessive adhesions (scarring) and tethering between different organs and surrounding tissues after mesh implantation can contribute to pain and can affect bowel/bladder function. This can create tension to nearby organs and tissues.
Steps to take when you start experiencing any of these symptoms
- Go back to your GP or implanting surgeon to discuss these.
- If you do not feel as though your questions were satisfactorily answered, ask to be referred to another surgeon to seek a second opinion, and if possible, also another.
- Ask your GP/surgeon to fill out an ACC45 and ACC2152 to lodge a claim with.
- Ask your surgeon/GP to lodge a complaint to Medsafe, if they are unable and you need help, ask where you can get assistance to do Further information on how to do this is provided later in this document.
- If you are under the care of other health professionals that you may feel more comfortable talking with, talk with them first and ask them for advice, however they will need to have a good knowledge of surgical mesh related symptoms and the appropriate care pathway that should follow.
Questions to ask your doctor if you are thinking about having a surgical mesh implant
- Do you have any written information that I can take away with me?
- Before signing the consent form on the day of the operation, will there be an opportunity to contact you with any questions I have regarding the operation?
- Can you explain all my possible treatment options including non-surgical options, surgical options using mesh, and surgical options without mesh?
- Why is mesh being suggested for me and what are the benefits over non mesh alternatives? What are the risks associated with using this mesh product?
- What are the benefits of alternative non mesh options being used instead of mesh?
- What brand of mesh will be used? What is the name of the device?
- It is important to keep a record of what has been implanted, ask to be provided written information on the brand, bar code and name of device.
- How many mesh operations have you performed?
- How many removals of mesh have you undertaken?
- How many complications have you come across? What types of complications have your patients had?
- What will my follow up care be like after the operation?
- What side effects can I expect after surgery and what side effects should I report to you?
- What happens if I experience symptoms in years to come?
- If there is a complication, will you be able to completely remove the device? What happens if it can’t be removed, what will that mean for me going forward?
- What happens if this surgery does not correct my problem?
- What are the long-term effects of having complications? How will these long-term complications impact on other body symptoms or organs?
- What is the management of these symptoms once they occur?
Questions to ask your doctor when discussing mesh removal
Seeking a second opinion is always a good idea to help you feel confident when making decisions regarding treatment. It is important to discuss with your surgeon the possibility of having a full removal of the surgical mesh device vs having a partial removal. It may not be possible to have your mesh removed completely, this is dependent on your individual case and the type of device implanted. Partial removal can make it difficult to remove the device at a later stage and may result in you having to undergo multiple procedures.
If your doctor is unable to remove the device fully, and this is what you would like, ask if they can refer you to someone who has the skills to achieve a complete explant.
This list of questions below may help you to think of other questions that are important for you in your individual situation. It helps to write down what you want to ask before you visit your surgeon, this will enable you to make sure you have covered everything you want to know. It is good to have someone with you as a support person. If not all your questions have been answered, or you think of other questions after you leave, contact the surgeon afterwards to follow up with anything else you want to know.
- How many mesh removals the surgeon has previously undertaken, partial or full? This is dependent on the surgeon’s surgical experience in mesh removal also whether they are credentialed to remove mesh from difficult areas such as the Sacral Promontory, obturator muscle, obturator fossa (bone).
- How much of the mesh will the surgeon remove; will they completely remove the implant or only what mesh is easily accessible?
- Check if the surgeon can remove the mesh where it has been fixated e.? staples, sutures, arms, anchors.
- How many surgeries will need to be done to remove my mesh? Will I need any other surgical repairs, and will this be done at the same time as the removal procedure?
- If having a partial removal, ask how much of the mesh will be left in place. Where will the mesh be cut back from? What are the associated risks of leaving a part of the device in the deep tissues?
- Depending on the type of mesh implanted you may be able to have a trans-labial ultrasound scan to ascertain exactly where the mesh Ask if this is possible and if available where you live.
- How many other surgeons will be involved during your mesh removal procedure, who is the primary surgeon?
- Is the surgeon able to fix the repairs without using mesh?
- How many native tissue repairs has the surgeon done and how regularly do they do them?
- Has the surgeon had any problems with native tissue repairs?
- Can the surgeon fix the repairs at the same time as the removal of mesh?
- How many patients improve, symptoms stay the same or get worse after mesh removals?
- Is there a possibility that I may become incontinent after removing the mesh?
- Do you think that I will need a urinary catheter to void after the operation and how long would this be for?
- Ask the surgeon to provide a photo and measurements of your mesh once it has been removed. This is beneficial if you must undergo further mesh removal procedures. You may be able to request that you take your mesh home with you, if this is what you want.
- You can request that your mesh is sent for testing- talk to your surgeon first about what they would be specifically testing for, so you have a good understanding of why this would potentially be needed.
Some surgeons will snip a mesh tape to release the tension if it has been identified as being too tight. This should only be done in acute circumstances. Sling division can make it much harder for a subsequent surgeon to remove mesh once the tape has been snipped (divided). This can also put the patient at risk of multiple surgical procedures further down the track. Trimming of mesh is not recommended as it only delays problems to a later stage.
ACC
You can get help from an ACC advocate after experiencing a surgical mesh adverse event to help you navigate the ACC system. Getting your treatment injury accepted by ACC and dealing with ACC can be difficult so asking for help is a good idea. Please do not fill out the claim form yourself, this needs to be done by a health professional. You can find a summary of ACC entitlesments in Appendix Two.
Independent advocacy and support
ACC guidelines on what ACC covers for surgical mesh injury
When your claim is lodged with ACC and your treatment injury has been accepted, you can ask for them to provide home help after your surgery and you are able to claim for other entitlements and supports.
How to lodge a complaint to Medsafe
It is really important when you are up to it, to report your medical device injury to Medsafe. This process is easier and Medsafe can help you with this. Contact details below.
“Anyone can report an issue associated with a medical device. An issue may relate to an adverse event, or a quality issue. Patients, caregivers, healthcare professionals and suppliers are all encouraged to lodge an adverse event report if an incident has occurred and there is a concern about the safety of the device or its use”.
Fill in as much of this form as you can and don’t worry if you don’t know everything. If you give permission at the end of the form, Medsafe will be able to contact the healthcare provider to request the additional information.
If you need assistance to complete this report please contact + 64 4 819 6800 to speak to a Medical Device Advisor.
How to Report a Problem to Medsafe
Consumer Form for Reporting an Adverse Event
